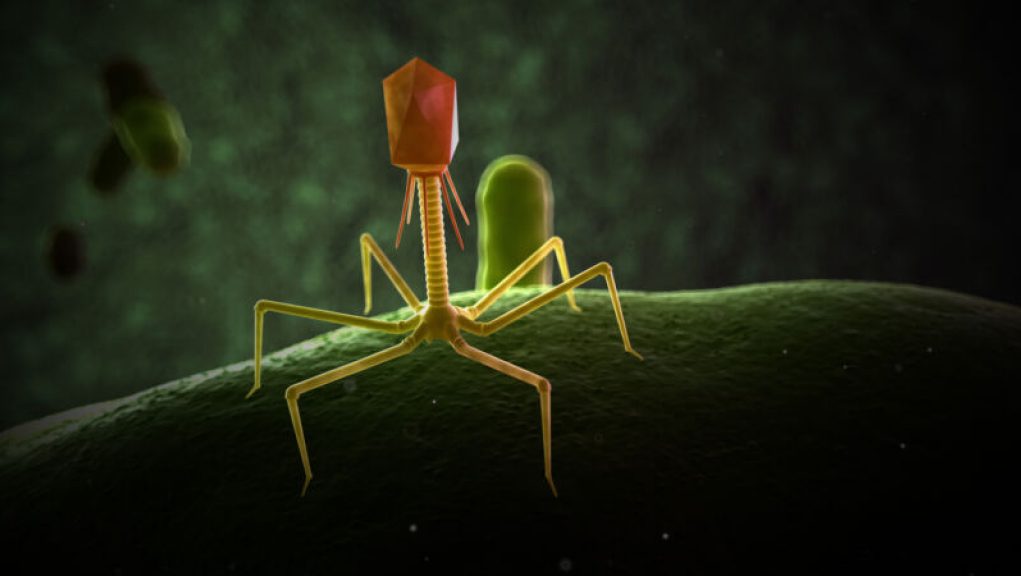
Are broad-spectrum antibiotics like nuclear bombs, destroying every prokaryote they come across? While they may be effective at eliminating pathogens, they’re not so great for maintaining a healthy microbiome. What we need are precision antimicrobials that can target only harmful bacteria while leaving the other species we need in our bodies to thrive. And that’s where SNIPR BIOME comes in. This Danish company is dedicated to engineering bacteriophages, viruses that target bacteria, to make them hyper-selective. Their first drug, SNIPR001, is currently in clinical trials and is designed for people with cancers involving blood cells.
Patients with these types of cancers often need chemotherapy, which can cause immunosuppression and increased intestinal permeability. This means they can’t fight off infections from bacteria that escape from their guts into their bloodstream. The mortality rate from such infections is around 15-20%, and many of them are caused by E. coli, much of which is already resistant to commonly used antibiotics.
SNIPR BIOME’s team screened 162 phages to find those that would infect a broad range of E. coli strains taken from people with bloodstream or urinary tract infections, as well as from the guts of healthy people. They settled on a set of eight different phages and engineered them to carry the genes that encode the CRISPR DNA-editing system. This approach has been shown to prevent the evolution of resistance.
After testing the ability of these eight engineered phages to kill the E. coli panel alone and in combination, they decided that a group of four of them was the most effective, naming the mixture SNIPR001. The team confirmed that SNIPR001 remains stable for five months in storage and does not affect any other gut bacteria.
SNIPR001 was well-tolerated in Göttingen minipigs and mice, reducing the amount of target E. coli in the feces without promoting drug resistance. SNIPR BIOME’s goal of using CRISPR to precisely target only harmful bacteria may revitalize phage therapy, allowing us to continue vanquishing our bacterial foes without promoting drug resistance.
In recent years, gene editing has become increasingly popular as a tool for studying and manipulating the genes of organisms. Recent advances have allowed researchers to modify viruses that are capable of killing bacteria, making them even more lethal.
The ability to modify viruses that target bacteria opens up a new realm of possibilities for fighting bacterial infections and diseases. These viruses, known as bacteriophages, have been used for decades to treat bacterial infections, but their effectiveness has been limited. By using gene editing techniques, scientists have been able to modify the DNA of these viruses to make them more effective against bacterial infections.
One of the main advantages of using gene editing for this purpose is that it allows researchers to precisely target specific genes that are responsible for causing a bacterial infection. This method of gene editing also gives researchers a better understanding of how bacteria react to these modified viruses, thereby allowing them to design more effective treatments for bacterial infections.
Gene editing has also enabled researchers to modify viruses that attack bacteria so that they can replicate more rapidly and kill more bacteria. This allows these modified viruses to act quickly and efficiently, reducing the amount of time a patient needs to stay in a hospital or receive antibiotics and other treatments.
All in all, gene editing has revolutionized the way scientists combat bacterial infections. By increasing the lethality of viruses that target bacteria, gene editing has made it possible to better control and treat bacterial infections with greater accuracy and precision.